
Virtual reality (VR) technology has become a prominent educational tool within the medical community, providing an immersive and risk-free laboratory environment for health care professionals. In the field of transfusion medicine, VR is being used to improve clinical competency, enrich the user’s learning experience and reduce reported errors within a controlled setting.
The United Kingdom’s NHS Blood and Transplant (NHSBT) has developed three virtual reality blood transfusion training apps to improve patient safety and increase awareness of transfusion medicine and biomedical science: one that utilizes ABO tile testing to convey basic principles of transfusion testing and ABO compatibility; one for crossmatching focused on procedural accuracy and background principles for biomedical scientists (BMSs); and a third for ABO testing by card agglutination technique (CAT) that focuses on practical skills and precise interpretation for BMS training.
“We feel that all these apps are interconnected and support one another. Long-term, we see them being linked together as part of a cohesive educational tool,” said Ruth Evans, scientific and clinical training and education lead for NHSBT.
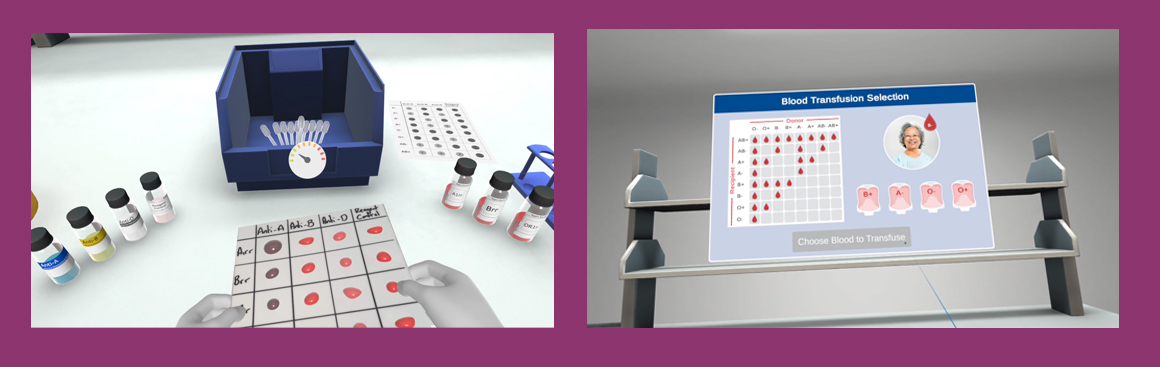
NHSBT’s first innovative VR training app, Blood Identification, simulates the process of an ABO blood group by tile technique with the aim of showing users how quickly agglutination of red cells can occur, in the test and within the body, reinforcing the importance of selecting the right blood group for transfusions. The handset replicates the sense of handling items such as blood samples and pipettes, engaging users throughout the process.
In the simulation, users enter a virtual transfusion laboratory, where they begin by testing a blood sample using reagents to determine the ABO blood group, then choose the correct red cell unit for transfusion, based on their ABO group results. After hanging a red cell unit at the patient’s bedside, they observe what happens in the bloodstream.
“You can watch the complement system activate and lyse the cells,” Evans said. “If you've made a critical mistake, you see the red cells being destroyed. If not, they circulate normally. And if the outcome is fatal, you hear a flatline.”
Although initially designed as a training tool for doctors, scientists and college students, Blood Identification has expanded its reach to a general audience and garnered interest from patients who routinely receive blood transfusions. One patient with thalassemia described the app as exciting and informative, and found it “reassuring to know blood is matched, safe and available.”
“We realized it was a much wider audience than we originally envisioned,” stated Eric Peotto, digital learning consultant, NHSBT. “We also learned that even patients found it helpful. It became an educational tool for people who wanted to understand what happens during a transfusion.”
The app also enacts potential complications within the environment, such as expired reagents. “The developers built in dynamic date ranges, as well as physics, to simulate the liquid moving, so you could assess whether the reagents still looked viable,” Peotto explained. “It aims to replicate, as closely as possible within the VR environment, the real-life decisions and critical moments that lab staff face during these processes.”
In 2023, Laura Eastwood, clinical scientist at NHSBT, set out to develop a VR app to enhance blood transfusion training for biomedical scientists and reduce errors in transfusion labs. According to the U.K.'s 2024 Serious Hazards of Transfusion (SHOT) annual report a 17.1% increase in laboratory errors was seen from 2023 to 2024. The most common category of transfused laboratory errors occurred at the testing step, with increasing gaps in laboratory staff knowledge identified in many cases.1
Eastwood emphasized that the increasing workload since the COVID-19 pandemic, staffing shortages and retirement of experienced staff have contributed to the widening knowledge gaps and ongoing challenges in providing hands-on training.
“Many of the incidents reported in the SHOT report stem from gaps in knowledge during the crossmatch phase,” Eastwood said. “Even though crossmatching is performed at the end of the transfusion process, it's often where the most issues arise, so we began exploring technology to improve training and support training officers.”
Eastwood and her team incorporated lessons learned from the Blood Identification app and worked closely with biomedical scientists from different hospitals, along with patient and donor stakeholders and transfusion-related regulatory bodies to design the NHSBT Crossmatching VR app with detailed clinical scenarios, including the treatment of sickle cell disease (SCD).
“We made a deliberate choice to include a patient with SCD in the app following the U.K. government’s Nobody’s Listening report, which highlighted serious gaps in care for this patient population, especially in hospitals that don’t regularly see hemoglobinopathy cases,” Eastwood said. She noted the crossmatch app addresses basic but critical care needs for patients with SCD with antibodies so that any lab can provide consistent, gold-standard care, regardless of experience.
“People may freeze or make mistakes because they simply don’t know what to do,” she added. “NHSBT provides blood for patients with SCD, and we believe it is our responsibility to support health care professionals with knowledge and resources in this area to ensure patients receive the best care.”
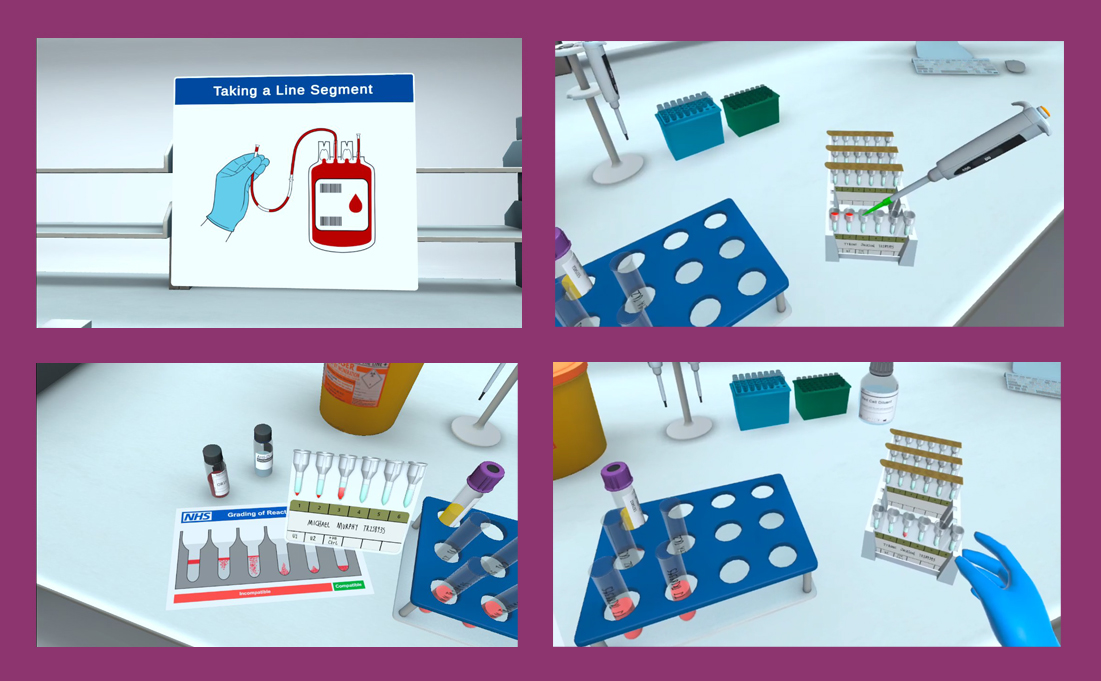
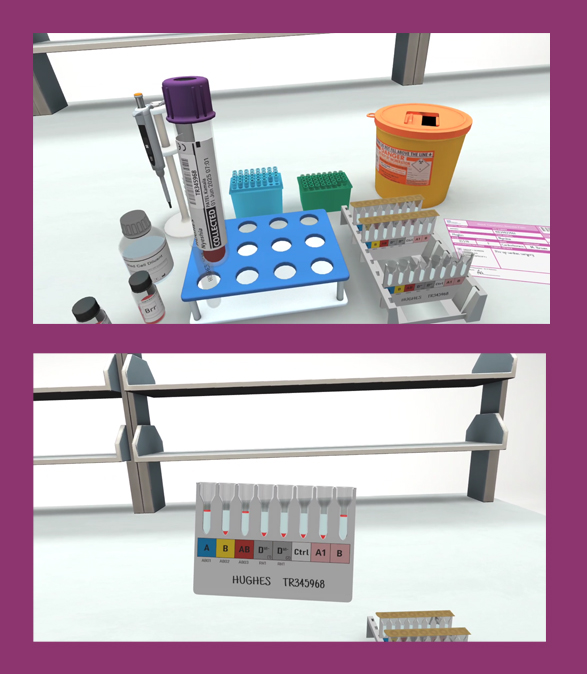
Created in collaboration with Make Real Ltd., the app, the first of its kind, simulates a crossmatch test in a virtual laboratory, enabling scientists to test blood samples, select compatible units and interact with virtual patients to understand the clinical context of their decisions. The scientist selects from three patient cases, each based on the most common errors reported in transfusion labs. Simulating the process in VR allows learners to practice and refresh their knowledge, without the use of valuable resources.
Research shows selecting expired or incorrect components or making errors in the crossmatch testing process can compromise the test results, with potentially fatal outcomes.2 Eastwood recalled a time when a health care professional, who was also a patient stakeholder in the app development, made a critical error in the app during the first trial. “He confused Jka with Jkb, which could be a life-threatening mistake in real life. He was shocked by the consequences and completely changed his perspective,” Eastwood said. “It really drove home how important even a small mistake can be, and how vital it is to train for that.”
After being piloted at Manchester Metropolitan University's School of Digital Arts in 2024, the Crossmatching app was trialed in approximately 50 hospitals and NHSBT blood centers across England and Wales. The findings demonstrated that VR training can be just as effective as in-person training.
“Many VR studies focus on perceived skill development, but ours included both perceived and observed skills,” Eastwood told AABB News. “Participants were initially skeptical, but the data showed that the practical skills they learned in the virtual laboratory did actually transfer to the real world. The results also suggested there was better retention and confidence at three months post-VR training.”
Procedural accuracy was also higher in the VR group—more than 90%—compared with 50–60% in the control group. Eastwood attributed this consistency to having standardized, distraction-free learning, noting that the haptic feedback, immersive experience and procedural repetition helped users feel prepared for real-life scenarios.
“We’ve also found that it reduces lab anxiety. Even medics said it made their first experience in the lab less intimidating,” Evans added. “VR training also helps reduce wastage. Training with real materials carries risks like expired samples, incorrect techniques and the potential for costly mistakes. VR offers a safe space to practice without consequences.”
Eastwood shared positive feedback from training officers regarding the use of VR over traditional training methods. Flexibility and adaptability were cited as key benefits among trainers. While traditional training requires reagents and other consumables, as well as potential travel expenses and accommodation, VR training can happen independently. For instance, if a trainer is based at a hub site but needs to support multiple spoke sites, VR headsets at those locations could potentially make training much easier.
“With the development of multi-user VR, trainees could be in different locations but still interact in the same virtual lab, or a facilitator can guide a larger audience through the training while someone participates in the VR environment,” Eastwood said. “This opens up new approaches to teaching and learning.”
Looking ahead, Eastwood hopes to expand transfusion VR training to include trauma and major hemorrhage scenarios. These high-pressure situations are ideal for VR training because they allow users to build muscle memory and decision-making skills in a safe, controlled environment, she pointed out. Moreover, training with distractions like ringing phones or urgent calls for blood in the background can prepare staff better than traditional setups.
“Long-term, we’d like to do a proper gap analysis to determine the most impactful training tools,” Eastwood said. “The goal is to create a patient journey in VR from start to finish, with multiple apps simulating each part of the process—then link them together into a complete experience,” she said.
“These are complex, high-stakes procedures, and VR helps staff feel like they've done it before, which builds confidence, reduces errors and improves outcomes for patients.” - Eric Peotto
Peotto noted the next five years of VR in transfusion medicine will be transformative. “We're only just beginning to see the impact VR can have,” Peotto said. “We've already started using it not just in transfusion but across NHSBT, including eye donation, heart and organ transplantation. These are complex, high-stakes procedures, and VR helps staff feel like they've done it before, which builds confidence, reduces errors and improves patient outcomes.”
NHSBT is leading the way nationally in applying VR in transfusion and transplantation, he told AABB News. As technology advances, the team will explore mixed reality and augmented reality to train staff within lab settings. “This isn’t just innovation for innovation’s sake—it’s meaningful, user-focused and based on evidence. The feedback, the outcomes and the user engagement have all been phenomenal,” Peotto said.
Both Eastwood and Peotto expressed their excitement about the future of VR in transfusion medicine and its potential to advance science and medical training. VR technology helps connect lab science to patient care in a more visceral way, Eastwood pointed out.
“That’s what makes VR so powerful,” Eastwood said. “It's not just for scientists—it helps patients understand their care better too. We’re breaking down the walls between labs, clinicians, and patients, and that shared understanding improves care across the board.”
PREVIOUS STORY
The Future of Transfusion Medicine and BiotherapiesBACK TO ISSUE
July 2025
Transfusion is AABB’s scholarly, peer-reviewed monthly journal, publishing the latest on technological advances, clinical research and controversial issues related to transfusion medicine, blood banking, biotherapies and tissue transplantation. Access of Transfusion is free to all AABB members.
Learn More About Transfusion Journal
Keep abreast of what's happening in the field of biotherapies with CellSource - AABB's monthly update on the latest biotherapies news.
To submit news about the blood and biotherapies field to AABB, please email news@aabb.org.
President
Meghan Delaney, DO, MPH
Chief Executive Officer
Debra Ben Avram, FASAE, CAE
Chief Communications and Engagement Officer
Julia Zimmerman
Director of Marketing and Communications
Jay Lewis, MPH
Managing Editor
Kendra Y. Mims, MFA
Senior Communications Manager
Drew Case
AABB News
(ISSN 1523939X) is published monthly, except for the combined November/December issue for the members of AABB; 4550 Montgomery Avenue; Suite 700 North Tower; Bethesda, MD 20814.
AABB is an international, not-for-profit association representing individuals and institutions involved in transfusion medicine, cellular therapies and patient blood management. The association is committed to improving health by developing and delivering standards, accreditation and educational programs that focus on optimizing patient and donor care and safety.
+1.301.907.6977
Email: news@aabb.org
Website: www.aabb.org
Copyright 2025 by AABB.
Views and opinions expressed in AABB News are not necessarily endorsed by AABB unless expressly stated.
Notice to Copiers: Reproduction in whole or part is strictly prohibited unless written permission has been granted by the publisher. AABB members need not obtain prior permission if proper credit is given.
