As the cord blood community addresses challenges, researchers examine why cord blood still matters.
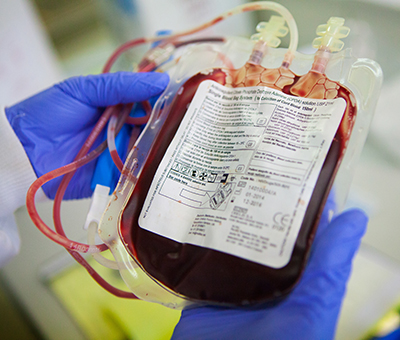
The use of cord blood to successfully treat life-threatening blood disorders dates to the 1980s, when a 5-year-old boy with Fanconi anemia received the world's first cord blood transplant.1 Cord blood has since evolved from a discarded medical waste into a curative option for the treatment of malignant and non-malignant diseases, including sickle cell disease and blood cancers.2
More than 60,000 cord blood transplants have been performed worldwide.3 Yet, despite growing value for diverse patient populations and emerging cellular therapies, cord blood is losing ground in stem cell transplantation. Annual reports from the World Marrow Donor Association show that worldwide cord blood shipments fell to 2,330 in 2023, down from 2,492 in 2022 and 2,783 in 2018.4
Filippo Milano, MD, PhD, an associate professor at Fred Hutchinson Cancer Center and the University of Washington, is also the scientific director of the cell therapy laboratory at Fred Hutchinson Cancer Center and the director of its cord blood program. He spoke with AABB News about the importance of cord blood for patients from diverse racial and ethnic backgrounds.
“With conventional stem cell sources—matched related or unrelated donors—80-90% of transplants go to patients of European ancestry. Minority patients are far less likely to find a match,” noted Milano. “In my cord blood program, 55% of recipients are from minority backgrounds. That is a dramatic shift. We analyzed our data and found that cord blood is often the best option for Hispanic and Black patients when a matched related or unrelated donor is not available. Cord blood provides access and equity in a way that other stem cell sources simply cannot.”
Milano also warned that the decline in cord blood collection could have long-term consequences.

“Our population is becoming increasingly diverse. Units collected 10 or 20 years ago will not represent the patients who will need transplants in the future. Stopping collection threatens the diversity that makes cord blood so valuable,” he said. “We also live in a world where unexpected events can disrupt donor availability, as we witnessed during the COVID-19 pandemic. If it becomes difficult to access unrelated donors, cord blood is immediately available. We should not take that for granted.”
Colleen Delaney, MD, MSc, vice president and chief medical officer of Seattle Children’s Therapeutics and an attending physician at Seattle Children’s Hospital, said cord blood must remain a viable transplant option for patients with blood cancers and minimal residual disease.
“In 2026, there should be a donor for everyone, whether that’s cord blood, matched unrelated, mismatched unrelated or haploidentical donors. We’re making advances across all donor sources, but we need to put the patient first and understand what their disease requires,” Delaney said. “There is a time and place for cord blood transplant, and in some cases, it may be preferred over other donor sources. Cord blood transplant must remain part of our armamentarium. It needs to remain an option.”
Multiple public blood banks have stopped collecting new cord blood units due to declining utilization and financial pressures. In 2020, the New York Blood Center, the world’s oldest public cord blood bank, closed its National Cord Blood Program.5
Milano noted that this decline is driven by falling demand. “In the U.S., there are fewer than 500 cord blood transplants per year, and there are even fewer in Europe,” he said. “The inventory is currently sufficient because demand is low. If cord blood were used more frequently, we would need a much larger and more diverse inventory.”
Delaney, a cord blood transplant physician and cellular therapy developer, discussed the significance of public banks for advancing new cellular therapies.
“Public banks collect material that’s essentially a snapshot in time. These units represent the population being born today – people who may require a transplant in the future,” Delaney said. “As our population becomes more diverse, these units become more precious because they may be the source of cells a patient matches with for a life-saving transplant. I strongly believe we need to continue supporting public collection because it’s so representative of the people who will need transplants tomorrow.”
Delaney, who has spent the past 25 years developing therapies derived from umbilical cord blood stem cells, said public banks are also vital for building the next generation of treatments.
“Our group was the first to show that you could expand stem cells in the lab and give them to a person, and their time to engraftment dropped dramatically because of the cells we were producing,” she said. “Today, we use cord blood to make adjuvant cellular therapy products—expanded stem cells that can be given in addition to a primary graft. In other words, what we make is not the primary donor source.”

Delaney said her team focuses on developing off-the-shelf products that do not require HLA matching. One of the unique advantages of cord blood, she mentioned, is that they can pool multiple cord blood units and expand their stem cells in a standardized way.
“From those expanded cells, we can direct them into immune effector cells, such as natural killer cells, or into myeloid cells that we can engineer,” Delaney told AABB News. “We’re developing engineered immune effector cell therapies derived from pooled donor cord blood, with the goal of treating solid tumors, liquid tumors, autoimmune disease and other conditions.”
She added that standardization, including the licensure and accreditation process, has made it easier for developers to work with qualified materials and navigate FDA regulations.
“Cord blood is an approved biologic therapy,” Delaney said. “There are approximately nine cord blood banks now with biologics licenses, so as a developer, it’s valuable to work with those banks because that material is already considered approved for clinical use.”
According to Delaney, public banks should be key partners in developing new therapies. “Cord blood is a pristine, highly workable source of starting material,” she continued. “And beyond stem cells, cord blood contains other valuable cell types. Companies are developing therapies using natural killer cells, regulatory T cells and other populations derived from cord blood. That’s why cord blood will become even more valuable as a starting material for future cellular therapies.”
One of the most important advances in cord blood banking has been the widespread adoption of red blood cell depletion. Today, most cord blood banks collect and process units this way, removing red cells to reduce variability and optimize storage.
“In the past, there was a huge amount of unpredictability in cord blood units, making it difficult to predict engraftment,” Milano said. “Now, because the units are more standardized, we can better predict how a patient will engraft. That has significantly improved outcomes, because historically engraftment was always the main challenge with cord blood.”
Milano and colleagues also established evidence-based thresholds defining optimal selection criteria for cord blood units based on total nucleated cells (TNC) and CD34 cell dose. Since publishing these guidelines, their findings report that graft failure has decreased dramatically, making engraftment far more predictable.6
“We are now seeing faster engraftment and lower non-relapse mortality when physicians follow these criteria,” Milano said.
Delaney added that this process has been translated directly to patient care, with most patients grafting by day 20, similar to bone marrow transplantation.
“When I first started doing cord blood expansion work, the goal was to get a patient to engraft before day 28,” she said. “Now, at least here in Seattle, it’s unusual to go beyond day 20 without engraftment in adult or pediatric patients, and we’ve done hundreds of transplants. That’s on par with bone marrow grafts using post-transplant cyclophosphamide, where engraftment may also occur around day 20 or later.”
“Even the best banking, storage and matching cannot translate into better patient outcomes if clinicians are not utilizing cord blood. Cord blood still produces excellent outcomes, especially for high-risk patients and patients from diverse racial backgrounds. The evidence supporting cord blood continues to grow, and we should not let it disappear.”
Delaney also noted improved outcomes for high-risk patients. “We’ve seen success using cord blood in patients with minimal residual disease. Cord blood can cure those patients, in some cases better than other stem cell sources,” Delaney said.
Milano agrees that unit quality and predictability have reached extremely high levels but warned that these advances only matter if cord blood continues to be used.
“I’d caution clinicians against abandoning something powerful just because it is harder to use,” Milano said. “Even the best banking, storage and matching cannot translate into better patient outcomes if clinicians are not utilizing cord blood. Cord blood still produces excellent outcomes, especially for high-risk patients and patients from diverse racial backgrounds. The evidence supporting cord blood continues to grow, and we should not let it disappear.”
Delaney addressed two common myths about cord blood transplant outcomes: delayed engraftment and graft failure.
“People still say it takes too long to engraft or graft failure rates are too high, but that’s not true anymore,” she said. “Multiple studies from multiple centers show outcomes are equivalent to other donor sources. There are pros and cons to each option, but cord blood is a very viable source of cells. Clinicians should not wait for the optimal adult volunteer donor because patients can die waiting. In my opinion, no patient in 2026 should die for lack of a donor.”
Both Milano and Delaney expressed optimism about the future of cord blood, not only as a transplant source but as a powerful cellular resource.
“I’m most excited about better understanding the biology of the cellular therapies we’re creating, so we can use these products earlier in a patient’s disease course,” Delaney said. “My hope is that as we establish safety and efficacy for cord blood-derived cellular therapies, we can move them earlier in the treatment timeline so that patients don’t need bone marrow transplant or stem cell transplant anymore. Cellular therapies are incredibly powerful, especially when derived from healthy donor cells rather than autologous cells from patients who may have already received chemotherapy and other treatments.”
 Looking ahead, Milano said he is most excited about having access to high-quality units that better represent the world’s diverse population. “Although times are difficult right now for cord blood transplantation, I do not believe the story is over,” Milano said. “Cord blood is not just a stem cell source. In the future, cord blood will be used not only for transplantation but also for gene therapy, immunotherapy and regenerative medicine. Ideally, transplantation itself will become less necessary as we develop better treatments. But cord blood as a source of cells will remain extremely valuable.”
Looking ahead, Milano said he is most excited about having access to high-quality units that better represent the world’s diverse population. “Although times are difficult right now for cord blood transplantation, I do not believe the story is over,” Milano said. “Cord blood is not just a stem cell source. In the future, cord blood will be used not only for transplantation but also for gene therapy, immunotherapy and regenerative medicine. Ideally, transplantation itself will become less necessary as we develop better treatments. But cord blood as a source of cells will remain extremely valuable.”
Milano said patient success stories and promising clinical results continue to motivate his work, even as enthusiasm for cord blood wanes.
“Many of my patients are from minority backgrounds, and cord blood gives them a chance they otherwise would not have,” Milano said. “When you see patients return to work and school and live their lives without major complications, it is incredibly rewarding. Cord blood gives patients an opportunity when no other donor is available. That is what brought me into this field, and it is what keeps me here. We can still improve the field and give patients better outcomes.”
BACK TO ISSUE
February 2026NEXT STORY
Strengthening Quality and Practice
Transfusion is AABB’s scholarly, peer-reviewed monthly journal, publishing the latest on technological advances, clinical research and controversial issues related to transfusion medicine, blood banking, biotherapies and tissue transplantation. Access of Transfusion is free to all AABB members.
Learn More About Transfusion Journal
Keep abreast of what's happening in the field of biotherapies with CellSource - AABB's monthly update on the latest biotherapies news.
To submit news about the blood and biotherapies field to AABB, please email news@aabb.org.
President
Meghan Delaney, DO, MPH
Chief Executive Officer
Debra Ben Avram, FASAE, CAE
Chief Communications and Engagement Officer
Julia Zimmerman
Director of Marketing and Communications
Jay Lewis, MPH
Managing Editor
Kendra Y. Mims, MFA
Senior Communications Manager
Drew Case
AABB News
(ISSN 1523939X) is published monthly, except for the combined November/December issue for the members of AABB; 4550 Montgomery Avenue; Suite 700 North Tower; Bethesda, MD 20814.
AABB is an international, not-for-profit association representing individuals and institutions involved in transfusion medicine, cellular therapies and patient blood management. The association is committed to improving health by developing and delivering standards, accreditation and educational programs that focus on optimizing patient and donor care and safety.
+1.301.907.6977
Email: news@aabb.org
Website: www.aabb.org
Copyright 2025 by AABB.
Views and opinions expressed in AABB News are not necessarily endorsed by AABB unless expressly stated.
Notice to Copiers: Reproduction in whole or part is strictly prohibited unless written permission has been granted by the publisher. AABB members need not obtain prior permission if proper credit is given.
